What are Insomnia and Sleep Disturbances?
Insomnia is the most common sleep disorder, characterized by difficulty sleeping for days, weeks or even months. It may include having trouble falling asleep, trouble staying asleep through the night or waking early and being unable to get back to sleep. Insomnia may also be caused by poor quality sleep, where you wake up feeling unrefreshed. [2]
Insomnia can be short term, caused by stress or changes to your schedule. When insomnia occurs at least 3 times per week lasting for more than 3 months, it becomes chronic insomnia. Chronic insomnia can be experienced by about 10% of adults but it is more common during perimenopause, with 40% to 60% of women experiencing difficulty sleeping. [2]
Insomnia has lasting effects into the day, causing lingering feelings of tiredness and/or “brain fog” – impaired brain function leading to memory loss, trouble concentrating and loss of ability to plan. Sleep loss caused by the environment (too much light or noise) is not insomnia.
Insomnia is a serious condition. Deep sleep is crucial for overall health and muscle and nerve repair. Lack of deep sleep due to insomnia increases headaches and inflammation. It can also lead to an increased risk for high blood pressure, cardiovascular disease, obesity, depression and other illnesses.
Insomnia in perimenopause is associated with an increased risk of neurodegenerative diseases including Alzheimer’s disease. [2] [3] [9]
For women in the menopausal transition, perimenopause insomnia and perimenopause sleep problems can be the main issue. [13] However insomnia is often a secondary condition caused by other symptoms such as hot flashes and night sweats, mood disorders, psychosocial factors, or other sleep disturbances such as obstructive sleep apnea (OSA) or restless legs syndrome (RLS). Insomnia and night sweats commonly occur together.
Estrogen and progesterone decline may be involved, as well as the sleep hormone melatonin . These hormones are involved in maintaining daily (circadian) biorhythms. [8]
Insomnia during perimenopause is often coupled with physical pain, chronic stress, anxiety, depression and/or hot flashes. Insomnia increases the risk of developing depressive symptoms during perimenopause by 2 to 3 times. [4]
Depression and insomnia are bidirectional: they reinforce each other, becoming a feedback loop – depression leads to insomnia, which leads to more depression, which leads to more insomnia, and so on. Similarly, chronic stress often increases anxiety, and both interfere with sleep. [3] [4]
Self-Care & Natural Remedies for Menopause Insomnia
It is important to seek medical help if insomnia lasts for a few weeks or more. A physician can help rule out any underlying health conditions that might interfere with quality sleep.
Menopause insomnia treatment is available. In fact you can also start by taking steps at home to address sleep issues, starting with improvements to your sleep hygiene.
➜ >Sleep in a cool, very dark room.
➜ Don’t look at bright lights before bedtime, especially those in the blue light range. While all visible light suppresses secretion of melatonin, blue light is particularly disruptive. Smartphones, televisions and computers emit in the blue light range, so minimize screen time on phones and computers 2 hours before bedtime.
➜ Keep a similar bedtime every day, and eat at regular times during the day.
➜ Avoid alcohol two hours before bedtime.
➜ Quit or cut back on smoking or other use of tobacco products, as nicotine is a stimulant also known to disrupt sleep.
➜ Melatonin therapy may help short term insomnia but may not help over the long term. Sunshine boosts melatonin production, and studies have shown an improvement in sleep with exposure to sunshine during the day.
➜ Exercise, particularly in outdoor daylight, to improve circulation and relaxation and to increase your natural sleep drive.
➜ Journal the events in your life to see how they correlate with insomnia.
➜ Some people find that meditation and mindfulness exercises before bedtime improves sleep.
➜ Shift work harms sleep quality, which is further disrupted during menopausal transition. Shift workers may need professional therapy to help with the combined effects of the menopausal transition and altered schedules.
Therapies & Treatments for Menopause Sleeping Difficulties
If you do not already have a healthcare practitioner who is familiar with identifying and treating symptoms of menopause, the North American Menopause Society provides a list of menopause practitioners here.

Medications + CBT
Anti-anxiety and anti-depression medications combined with psychological counseling may be very helpful. Cognitive Behavioral Therapy (CBT) is a short-term therapy technique used to alter behaviours by changing thought patterns which has been shown to be quite effective for insomnia. [1]

Melatonin
Supplements of melatonin, the ‘sleep hormone’, has been shown to be effective in helping women fall asleep and stay asleep during perimenopause. Melatonin levels naturally decline with age, and this decrease is happening during the menopausal transition years. [5] [6]

Ramelteon
Ramelteon is a molecule that helps produce melatonin. When it is given as a sleep aid, it has been shown to increase total sleep time and it helps with falling asleep. It is not yet available in Canada. [5]

Agomelatine
Agomelatine is an antidepressant medication that boosts melatonin production. It can be effective as a treatment for co-occurring insomnia and depression. Caution is needed as this medication can damage the liver. [5]

Hormone Therapy
Decreasing levels of estrogen and sleep disturbances do not appear to be directly linked. However, hormone therapy (HT) can be effective at treating night sweats that can be the primary cause of insomnia for some women. Hormone therapy with estrogen may be helpful for preventing short-term memory loss and minimizing sleep loss resulting from hot flashes and night sweats.

Physiotherapy
Physiotherapy may be able to help sleep quality by decreasing physical pain and increased mobility.

Check for Obstructive Sleep Apnea
Check if you (or your bedmate) have obstructive sleep apnea (OSA), characterized by snoring, gasping or disrupted breathing while asleep. Apnea can be dangerous, so consult a physician if you suspect it may be a contributing factor.
Female night shift workers need to be vigilantly screened for breast cancer, as they have a 48% increased risk for developing breast cancer. This is because melatonin, a hormone involved in regulating sleep is also known to suppress breast cancer tumours. [6]
Statistics
Insomnia and disrupted sleep during menopause can have short- and long-term impacts on overall health and quality-of-life.
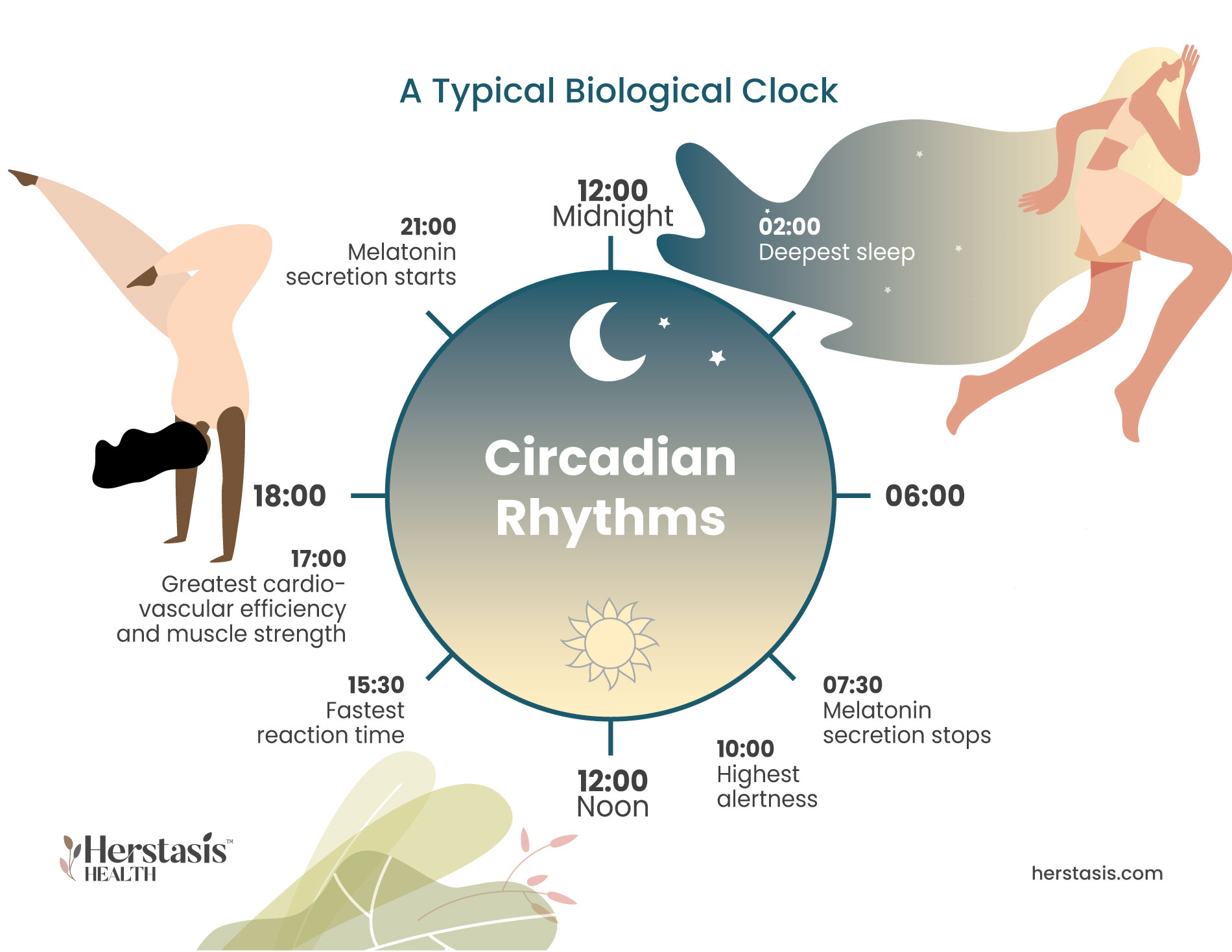
Typical Biological Clock
Biological clocks are rooted in biochemistry and gene functions, and control all aspects of body and brain function. Human biological clocks follow a circadian cycle: an intricate daily rhythm of interactions in genes, cells, tissues, and behavior.
Two brain regions, the hypothalamus and suprachiasmatic nucleus, regulate sleep and waking circadian cycles, and are sensitive to fluctuations and decreases in estrogen and melatonin that happen during perimenopause and postmenopause. This may cause disruption of sleep.
Melatonin, a hormone secreted by the pineal gland at night, primes the brain and body for rest and repair at night. Melatonin secretion may be affected by fluctuations and declines in estrogen and possibly progesterone. [6]
The Stages of Sleep
Sleep is a period of rest that alternates with wakefulness. During sleep, your body conserves energy and cells resupply their energy stores, as well as works to heal any injuries or repair any tissues that need it, such as muscle tissue after working out. Sleep is also the time when your body can do its regular maintenance activities, including cataloging memories and storing learned information. [11]
Once asleep, you cycle through the stages of sleep throughout the night in a predictable pattern. [10] Sleep cycles involve two main types of sleep – rapid eye movement (REM) and non-REM sleep (NREM). One full sleep cycle usually lasts between 1 to 2 hours.
There are 3 non-REM stages:

Stage 1
Stage 1 is when you enter into a light sleep. This is the shortest stage and lasts only a few minutes. Throughout the night and your sleep cycles you will spend about 5% of your time in this stage.

Stage 2
Stage 2 is a deeper sleep and the longest stage (combined through different cycles), as you spend about 45% of your sleep in stage 2. When you enter stage 2 NREM sleep, your blood pressure and heart rate fall because they aren’t needed to control your body as much as when you are awake. Your brain activity also slows down, with occasional spikes of brain activity. The hypothesis is that this is the time when your brain works to organize and store the information you learned throughout the day, including storing memories.

Stage 3
Stage 3 is deep sleep, also called slow-wave sleep, named for the type of brain activity seen during this stage. This is the deepest stage of sleep and you will spend about 25% of your night in this NREM stage. During stage 3, any repairs to your body and brain occur and your immune system is strengthened. This stage of sleep is hard to wake up from, and if you are wakened, you might be confused for up to 30 minutes. [11]
REM sleep is when dreaming happens. Your eyes move and your muscles may twitch although they are typically limp enough that you don’t carry out the movements in your dreams. Brain activity during REM sleep is similar to brain activity when you are awake. REM sleep makes up about 25% of your night’s sleep. [11]
Your body has a biological need for sleep that increases when you have been awake for a long time. This is controlled by a process called homeostasis, which is what maintains all your body systems in a steady state.
A compound called adenosine is linked to this need for sleep. While you are awake, the level of adenosine in your brain continues to rise. The rising levels signal a shift toward sleep. Caffeine and certain drugs can interrupt this process by blocking adenosine. [10]
The impacts of a lack of sleep include:
-
◇ slowed reflexes
◇ problems thinking and concentrating
◇ irritability
◇ depression
◇ headaches
◇ weakened immune system
◇ impulsive or reckless behaviour
◇ feelings of fatigue and exhaustion
Sleep is necessary to properly function. If you go for too long without sleep, you may experience microsleeps, which is when your brain falls asleep for a few minutes. This can be extremely dangerous if it happens while driving or using machinery. You may also experience tremors, as your nervous system will have trouble regulating your muscles and their movement.
Long-term sleep deprivation can cause hallucinations and psychosis, as your brain fails to properly interpret what is happening around you. In very rare cases, sleep deprivation can lead to death. [11]
Obstructive Sleep Apnea
Obstructive sleep apnea (OSA) is a condition where a blockage or narrowing in your airway keeps air from moving through your throat when you’re asleep. When this happens, the levels of oxygen in your blood drop, triggering a reflex that wakes you up just enough to take a breath. This can greatly interfere with your sleep and keep you from experiencing all the stages of sleep you need for optimal health.
Snoring while asleep, frequent waking episodes or feeling like you’re choking in the night are all symptoms of OSA. You may find you wake up with headaches, have difficulty focusing and concentrating and experience fatigue and exhaustion during the day.
Treating OSA is done using a continuous positive airway pressure, or CPAP machine. This machine uses air pressure, delivered as continuous air flow through your mouth and nose, which keeps your airways open. [14]
MYSTERY
Insomnia is a very common condition in modern life and is caused by environmental, social and biological factors. Research is actively trying to untangle the complex outcomes of these interactions.
FALSE
TV may be boring, but bright light and blue light can disrupt melatonin release and biological clocks.
FALSE
No, insomnia is common, and as a result there are many helpful therapies and self-care actions available to address it.
FALSE
At first alcohol is relaxing, but it actually interferes with the brain and body’s ability to sleep deeply and for long periods.
[1] Caretto, M., Giannini, A., and Simoncini, T., An Integrated Approach to Diagnosing and Managing Sleep Disorders in Menopausal Women.Maturitas, Volume 128, October 2019, Pages 1-3
[2] https://www.nhlbi.nih.gov/health/insomnia
[3] Brinton, R. D., Yao, J., Yin, F., Mack, W. J., & Cadenas, E. (2015). Perimenopause as a neurological transition state. Nature reviews. Endocrinology, 11(7), 393–405. https://doi.org/10.1038/nrendo.2015.82
[4] Caruso, D., Masci, I., Cipollone, G., & Palagini, L. (2019). Insomnia and depressive symptoms during the menopausal transition: theoretical and therapeutic implications of a self-reinforcing feedback loop. Maturitas, 123, 78–81. https://doi.org/10.1016/j.maturitas.2019.02.007
[5] Jehan, S., Jean-Louis, G., Zizi, F., Auguste, E., Pandi-Perumal, S. R., Gupta, R., Attarian, H., McFarlane, S. I., Hardeland, R., & Brzezinski, A. (2017). Sleep, Melatonin, and the Menopausal Transition: What Are the Links? Sleep Science, 10(1), 11–18. https://doi.org/10.5935/1984-0063.20170003
[6] Toffol, Elena MD; Kalleinen, Nea MD, PhD; Haukka, Jari PhD; Vakkuri, Olli PhD; Partonen, Timo MD, PhD; Polo-Kantola, Päivi MD, PhD. Melatonin in perimenopausal and postmenopausal women: associations with mood, sleep, climacteric symptoms, and quality of life. Menopause 21(5):p 493-500, May 2014. | DOI: 10.1097/GME.0b013e3182a6c8f3
[7] Pacheco, D. (2020, October 16). Shift Work Disorder Symptoms. The Sleep Foundation. https://www.sleepfoundation.org/shift-work-disorder/symptoms
[8] Lockley, S. W., Brainard, G. C., & Czeisler, C. A. (2003). High sensitivity of the human circadian melatonin rhythm to resetting by short wavelength light. The Journal of Clinical Endocrinology and Metabolism, 88(9), 4502–4505. https://doi.org/10.1210/jc.2003-030570
[9] Sabia, S., Fayosse, A., Dumurgier, J. et al. (2021). Association of sleep duration in middle and old age with incidence of dementia. Nature Communications, 12(2289). https://doi.org/10.1038/s41467-021-22354-2
[10] https://www.nhlbi.nih.gov/health/sleep
[11] https://my.clevelandclinic.org/health/body/12148-sleep-basics
[12] https://my.clevelandclinic.org/health/diseases/24443-obstructive-sleep-apnea-osa
[13] https://womenlivingbetter.org/sleep-disruption-in-perimenopause/
[14]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5776689/
[15] https://pubmed.ncbi.nlm.nih.gov/27760083/
Original content, last updated February 6, 2025.
© 2025 Herstasis® Health Foundation