Men can be deeply affected by a variety of changes to their bodies and minds that start during their midlife (40’s and 50’s). Night sweats in men and hot flashes in men are relatively common. Three different underlying physical and chemical processes – a mid-life crisis, male menopause, or andropause – may be the root cause for these changes. Read on to understand what these are, what the most common symptoms are, and how to manage the impacts of these symptoms.
What is Male Menopause?
Manopause. Male menopause. Midlife crisis. Andropause.
These terms are used interchangeably in the marketplace, and are confusing because men do not have the same drastic fluctuations and changes in sex hormones that underlie the female menopause.
Yet, enough men aged 40 – 60 experience significant emotional and physical changes during this time period that there does need to be a name for this stage of life. This will allow men to start to talk openly with their family and employers about their challenges, overcome stigma, and seek medical help when appropriate.
Andropause is a true medical condition, often caused by injury, disease or medication, but there is overlap between the symptoms of andropause and midlife, so we will use the terms “male midlife” and “male midlife crisis” to recognize the significance of the male experience of aging without confusing it with hormonal condition.
What is the Male Mid-life Crisis?
A mid-life crisis is a relatively common experience in men, and it can be an extremely chaotic and tumultuous time. A ‘typical’ midlife crisis is defined as a period or phase of life, usually between the ages of 40 and 60, when a man begins to question their accomplishments or achievements in their lives to date. While ‘crisis’ is the common term used for this experience, in fact it is a natural process that can, in the best case scenario, include re-assessment, adjustment and acceptance. A midlife crisis can also be a factor contributing to male menopause. [1] [2]
Signs you may be experiencing a midlife crisis as you turn 40 or older include:
▢ Experiencing general dissatisfaction with life, or questioning your existing life choices
▢ A sense that your best days are behind you, that it’s all ‘downhill’ from here
▢ Feeling trapped in your life
▢ Feeling torn between responsibilities to be breadwinner and losing time to spend with children
▢ Experiencing a sense of running out of time to make any life changes or life decisions
▢ Increasing mood swings or mood changes
▢ Increasing anger at the world in general for being unfair
▢ Increasing anger at specific individuals (such as bosses or family members) that you perceive to have held you back or been unsupportive
▢ Withdrawing from work, family, and life in general
[1] [3]

▢ Exhibiting changes in behaviour, especially destructive ones like:
◇ Starting or wanting to start an extra-marital affair
◇ Spending money on atypical items (like a sports car or a new boat)
◇ Spending money recklessly and/or beyond your means
◇ Leaving or wanting to leave your family
◇ Taking up high-risk sports and hobbies like sky-diving or rock climbing
◇ Having more focus on and changing your appearance, by changing the way you dress
◇ Significantly increasing your workouts, or considering (or having) cosmetic surgery
◇ Dropping long-time friends and relationships
When Will My Mid-Life Crisis Go Away?
It is possible to come out of your mid-life crisis better and happier than when you went into it because a mid-life crisis leads to either ‘growth or destruction’.
Growth happens when the underlying causes of unhappiness and dissatisfaction are considered, and you make careful and thoughtful decisions and plans to change and address those causes.
Unfortunately, you may come out of your mid-life crisis much less happy and satisfied than when you went in if you follow the destruction path. This happens when poor choices and not enough positive actions result in big changes such as leaving your family or spending money beyond your means. These destructive choices may feel like they are going to improve your life and your circumstances in the moment, but instead they often destabilize your life and remove carefully built community support systems.
[2] [4]
What Are Male Mid-life Symptoms?
Men experience real and sometimes debilitating physical and mental midlife symptoms, although they may not always report these to their healthcare provider immediately. These symptoms often interfere with day-to-day life and impact not just the men experiencing them, but also their friends, family and co-workers.
The most common symptoms include:
▢ Depression
▢ Loss of sex drive
▢ Erectile dysfunction
▢ Male pattern baldness
▢ Mood swings and irritability
▢ Anger
▢ Loss of muscle mass and reduced ability to exercise
▢ Fat redistribution, such as developing a large belly or “man boobs” (gynaecomastia)
▢ A general lack of enthusiasm or energy
▢ Difficulty sleeping an/or or increased tiredness
▢ Night sweats
▢ Hot flashes
▢ Poor concentration and short-term memory challenges
If you are experiencing any of these, talk to your healthcare provider so you can work with them to find the underlying cause(s) and find solutions that work for you. [5][6][7]

Andropause & Late Onset Hypogonadism Learn More

Male Menopause & Manopause Learn More

Erectile Dysfunction Learn More

Decreased Libido Learn More
Male Pattern Baldness Learn More
What are Andropause and Late Onset Hypogonadism (LOH)?
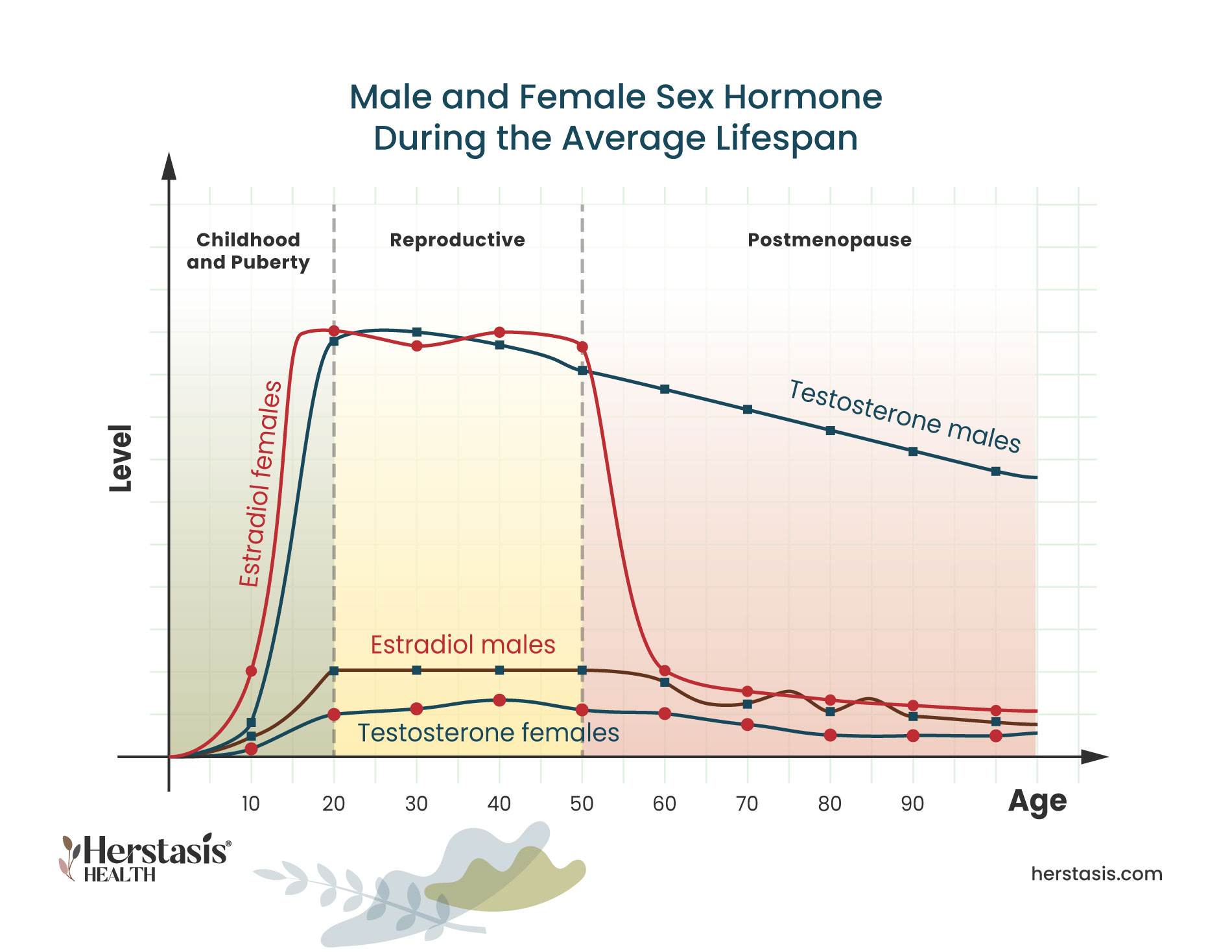
Testosterone, the main male sex hormone, goes through a slow, steady and progressive drop at a rate of about 1% per year starting in men’s 30s and 40s. This is not a medical condition, rather it is a normal and natural part of aging. The rate of decline in testosterone levels varies in different individuals and it can be affected by chronic disease, excess weight, illness, serious emotional stress, and medication side-effects. This natural rate of testosterone decline can be slowed (but not stopped) by making changes to lifestyle and behaviours.
Andropause is a medical condition that exists when there are no or extremely low testosterone levels. This is called hypogonadism and it occurs when the testes produce few or no hormones. It can be present from birth, which can cause symptoms like delayed puberty and small testes.
Hypogonadism can also occasionally develop later in life, known as late-onset hypogonadism (LOH), and it is most common in men who are obese or have type 2 diabetes. When this occurs, it can cause ‘male menopause’ symptoms. It is important to realize though, that LOH is a specific medical condition, not a normal part of aging. LOH may be responsible for some male midlife symptoms, but many symptoms are not associated with hormones at all. [5] [6] [7] [8]
What is Erectile Dysfunction?
Erectile dysfunction (ED) is defined as experiencing difficulty achieving and maintaining an erection sufficient to participate in sexual activity. Erectile dysfunction can be very hard to accept but there are ways to manage and overcome this symptom. Many men don’t seek or delay getting help because they are embarrassed. Don’t be! Ongoing ED severe enough to be reported to a physician affects over 30 million men in the US alone. Additionally, erectile dysfunction does happen to almost every man at some point in their lives. [9]
The penis contains two sponge-like structures called the corpora cavernosa. These are basically two cylinders that extend the length of the penis. Sexual arousal causes increased blood flow to both of these cylinders and the influx of blood causes an erection by expanding, straightening, and stiffening the penis. [10]
The causes of ED can be physical or they can stem from emotional and psychological issues.
The physical causes of ED include:
◇ Not enough blood flow to the penis. This can happen for a number of reasons including heart and cardiovascular disease, diabetes (which can cause small blood vessels and/or nerve damage), and smoking.
◇ The penis cannot hold available blood. If blood doesn’t stay in the penis, erection isn’t possible.
◇ Nerve signals from the brain or spinal cord do not reach the penis. This can happen as a result of some diseases, injuries, or nerve damage in the pelvic region.
◇ Surgery and or radiation for cancers in the lower abdomen or pelvis. ED is a common side effect of prostate, colon-rectal or bladder cancer treatments.
◇ Other medications used to treat other health problems.
Emotional and psychological causes of ED include:
◇ Depression
◇ Anxiety
◇ Relationship problems
◇ Stress
◇ Lack of self-confidence about sexual performance.
If you have a partner going through the menopause transition who has a diminished interest in sex, feelings of inadequacy and frustration can take over, causing issues for your own sexuality. Women taking medications for depression or anxiety may also experience a loss of libido or inability to orgasm which can be frustrating for both of you.
What can I do about ED?
Knowing the likely cause(s) of ED is the key to resolving it with the correct therapy. Physical treatments will use medications – either new ones or adjusting and/or changing your existing ones. You may also need to make lifestyle changes that include improving your nutrition, getting adequate sleep, and increasing your movement and activity levels.
If the causes of ED are emotional or psychological, talk therapy, meditation, and/or breathing exercises can help. The vacuum constriction device discussed earlier in this section is safe and has few long-term side effects. Because of this, it may be prescribed for use when the cause of ED is psychological. This is not a permanent solution, but will allow for successful intercourse while other treatments such as counselling, are ongoing. Talk to your healthcare provider to find a solution that works for you. [10] [11] [12]

Vacuum Constriction Device
In some cases, men may be prescribed a vacuum constriction device (VCD), also known as a penis pump. This device is an external cylindrical pump that is placed over the penis. Air is pumped out of the cylinder it creates a vacuum, and this vacuum draws blood into the shaft of the penis. The blood will cause the penis to swell and become erect. Once the erection is achieved, a retaining band is placed at the base of the penis to hold the blood in. The pump is removed and the band can safely stay in place for up to 30 minutes, allowing for intercourse. Use of the VCD will cause an erection, but there are differences when compared to a natural erection. Side effects from using the pump include a purplish colour to the penis, numbness, bruising and swelling of the penis and difficulty achieving orgasm. Additionally, ejaculation is unlikely and the penis will be cold. Warm compresses can be used to increase the penis temperature before intercourse. [11]
What is Decreased Libido or Decreased Sex Drive?
A decrease in your libido means you have a lowered sex drive, reducing your desire to have sex. You will have less frequent sexual thoughts and fantasies and you may engage in sexual activity less frequently. When libido is low, sexual stimulation can fail to cause interest.
Libido is not usually associated with the ability to achieve an erection, so men with a low libido can still engage in sexual activity to satisfy their partner.
Having to do this, however, may impact your overall relationship with your partner and can also have significant psychological effects for you. [13]
There is no ‘typical’ level of libido, and sex drive varies among men. As men age, there is a tendency to see a gradual decrease in libido, but age-related changes are gradual, if at all. Fatigue, anxiety, stress, or other conditions may cause temporary reductions in libido and this is normal throughout a man’s life. When noticeable changes to your libido develop after years of ‘normal’ levels of sexual desire, this can be very disruptive to relationships, and can also affect your self-esteem.
Psychological factors are often the root cause:
◇ Long-lasting depression
◇ Anxiety
◇ Alcoholism
◇ Illicit drug use
◇ Chronic fatigue
◇ Relationship stress
Physical factors can include:
◇ Chronic kidney disease
◇ Some prescription drugs, including those used to treat:
- Depression
- Anxiety
- Advanced prostate cancer
Treatments for Low Libido or Decreased Sex Drive
Treatment for low libido depends on the root cause. Treatments for psychological and emotional issues include talk therapy (such as cognitive behavioural therapy), as well as self-care practices. These include practicing meditation and/or breathing exercise, journaling your thoughts and feelings, joining a support group or a peer group and/or practicing Mind Body Wellness therapies. Mind Body Wellness therapies include: yoga, biofeedback and relaxation therapy, hypnosis, aromatherapy, meditative movement such as Tai Chi or Qigong. You may get inspired to try one or more of these and see if it helps any of your symptoms. [5]
A blood test can measure the level of testosterone in the blood. If this is the root cause of a low libido, it can be treated with testosterone replacement therapy (TRT).
Androgenic alopecia, known as male pattern baldness (MPB), is a benign type of hair loss that affects men. Male pattern baldness usually starts with thinning hair and a receding hairline that progresses to complete or near complete loss of hair on the scalp. Hair loss on the crown of the head usually appears in a circular shape. A receding hairline often occurs in an “M” shape. As you continue to lose hair, hair loss around your crown and temples may meet to form a “U” shape. Male pattern baldness happens over years. [15][16]
Male pattern baldness affects two-thirds of men. The early signs of MPB (hair thinning) may be seen as early as late teens or early 20s although typically it is noticeable by age 30. By age 50, half of the male population experience hair loss. [15]

Causes of Male Pattern Baldness
Male pattern baldness happens when your hair follicles (where the base of your hairs connect to your scalp) gradually shrink. A hormone called dihydrotestosterone (DHT) is a male sex hormones present in men and women. Hair follicles are sensitive to DHT, which can cause the follicle to ‘miniaturize’ and also cause a shortened hair growth cycle. As this happens the individual hairs get thinner and shorter. Over time, those hairs stop growing at all. [15] [17]
Impacts of Male Pattern Baldness
Male pattern baldness is a benign condition, meaning that there are no long term physical health implications. However, there are significant psychological impacts. For example, men suffering from hair loss:
- Worry about a loss of physical attractiveness
- Perceive a loss of social attractiveness
- Have drastically reduced body image satisfaction
- Increased cognitive preoccupation in more than 30% of men
- Are afraid that others will notice
- Worry about looking older than their actual age
- Feel hopeless about their hair loss
- Fear getting teased by their peers
- Have significantly more body image dissatisfaction than men with no hair loss
- Experience anxiety
- Experience helplessness
- Have diminished self-esteem
- Are self-consciousness
- Are embarrassed
- Feel frustrated
- Feel less virile
are jealous (of men with hair) - Feel physically and socially less attractive
experience a decline in quality of life
[17] [18]
Among males experiencing male pattern baldness:

find their condition to be extremely upsetting [17]

express some to moderate emotional distress [17]
Treatments for Male Pattern Baldness
There are treatments for male pattern baldness:
Causes of Male Mid-Life Symptoms
It can be difficult to pin down the exact reasons for men’s midlife symptoms. Low testosterone is often blamed, but it is rarely the primary cause unless there is a clear illness or injury to explain lowered hormone levels. Given this, it is important to recognize that lifestyle choices can be a factor, as well as psychological issues. For example, erectile dysfunction can result from stress, depression, and/or anxiety, but it is also associated with obesity, smoking, excessive drinking, and cardiovascular health problems. [5]
Common causes of male menopause symptoms include:
- ◇ Stress
◇ Anxiety
◇ Lack of sleep
◇ A poor diet
◇ Lack of exercise
◇ Drinking too much alcohol
◇ Smoking
◇ Low self-esteem [5]
Night sweats in men can be caused by low testosterone, but more commonly results from anxiety and/or stress, diet, alcohol, medications, or a side effect of sleep apnea. This is true of hot flashes during the day in men as well, where the most common causes are anxiety, stress, or side effects of medication. [21][22]
Self-Care & Natural Remedies for Symptoms of Male Midlife Crisis and Male Menopause
It is important to understand the root causes for any symptoms you may be feeling. Know that midlife is often a time of self-reflection and self-assessment, both of which can play an important role in symptoms experienced for midlife men. Self-care for your symptoms can play an important role in helping reduce their impact, regardless of the causes.

Talk to someone you trust.
Sometimes just sharing your experiences provides some perspective and can lower your anxiety or stress.

Take care of your physical body.
When you eat well, get adequate exercise, and have good quality sleep, you will feel better.

Exercise with friends.
Make connections with people while you are doing something good for your body and make it a regular thing you look forward to.

Practice meditation and/or breathing exercises.
Daily breathing or meditation practices help calm your mind and give you a smart tool for reducing the strength of mood swings, anger, depression or other behavioural symptoms in the moment they happen.
Journal your thoughts and feelings
Not only is keeping a journal a proven way to self-reflect and practice self-care, your journal can also help you track your symptoms. You may start to see patterns and identify situations that trigger uncharacteristic feelings and behaviours. Take the time to journal things that are good as well! This can be a boost when you are feeling down or irritated.
Join a support or peer group.
Your healthcare provider can give you a recommendation for a support group or point you to specialty care organizations that provide support for midlife men.
Therapies & Treatments for Symptoms of Male Midlife Crisis and Male Menopause
If you’re experiencing symptoms that could be caused by male menopause, see your healthcare provider. You will get tested for hormone levels, and you can also expect to discuss your work and personal life to see if your symptoms may be caused by problems such as stress, anxiety, poor sleep, or excess weight.
The Science
Testosterone can be found circulating in the body in ‘free’ form, where it is on its own, or it can be circulating in a form where it is ‘bound’ to proteins. About 98% of the body’s testosterone is bound to either SHBG (sex-hormone binding globulin), or to the protein albumin. Only 2% of the body’s testosterone is found in free form. Total testosterone, also called total serum testosterone, measures all testosterone in the blood, both free and bound forms. Free testosterone levels are significantly correlated with libido, erectile, and orgasmic function.
Testosterone is measured in units of nanomoles (nmoles) per litre (L). A mole is an amount of a substance that contains a very large number (6 followed by 23 zeros) of molecules or atoms. A nanomole is one-billionth of a mole. A litre measures fluid volume. Testosterone can also be measured in nanograms (ng) per deciliter (dL). A nanogram is one-billionth of a gram (which is about 1/30 of an ounce) and a decilitre measures fluid volume that is 1/10 of a litre.
There is general agreement amongst various professional bodies that total testosterone levels above 12 nmol/L (350 ng/dl) does not require testosterone supplementation. There is also a consensus that patients with total testosterone levels below 8 nmol/l (230 ng/dl) will usually benefit from testosterone treatment. If the total testosterone level is between 8 and 12 nmol/l (230 and 350 ng/dl) the tests can be repeated to look only for free testosterone. This measure will help determine whether or not the individual needs additional testosterone added to their system. [6]
No. The term is used in the media as a ‘cutesy’ way of describing symptoms that commonly occur to men starting in midlife. These symptoms overlap with symptoms commonly experienced by women during the menopausal transition but they do not have the same hormonal basis in men as they do in women.
Andropause is a condition that results from low to no levels of testosterone. Men can be born with this condition or it can develop throughout their lives from illness or injury. Andropause can also start in later life, when it is called late onset hypogonadism (LOH).
Male menopause, on the other hand, is a term used to describe symptoms that men start to show in midlife, including sexual changes and mood swings. Male menopause is not related to low testosterone levels seen in andropause. There is overlap in symptoms, causing some confusion.
No. Many men do get midlife symptoms around the same age that women start to get symptoms of perimenopause, the underlying hormone processes are not at all similar. In women, estrogen,the main female sex hormone, begins an abrupt decline that settles into steady but low levels that will persist throughout their lives. In contrast, testosterone, the main male sex hormone, goes through a slow, steady and progressive drop at a rate of about 1% per year starting in men’s 30s and 40s.
The roots of most male male menopause symptoms are usually related to lifestyle and behaviour problems. The first step for men experiencing symptoms in midlife is to check their testosterone levels in case that is a factor. But typically lifestyle changes such as improving diet, sleep, and exercise habits as well as treatment for any anxiety, stress or depression will help manage or even correct the symptoms.
The most common andropause symptoms include:
- depression
- loss of sex drive
- erectile dysfunction
- mood swings and irritability
- anger
- loss of muscle mass and reduced ability to exercise
- fat redistribution, such as developing a large belly or “man boobs” (gynaecomastia)
- a general lack of enthusiasm or energy
- difficulty sleeping an/or or increased tiredness
- night sweats
- hot flashes
- poor concentration and short-term memory challenges.
The most common male menopause symptoms include:
- depression,
- loss of sex drive,
- erectile dysfunction
- mood swings and irritability
- anger
- loss of muscle mass and reduced ability to exercise
- fat redistribution, such as developing a large belly or “man boobs” (gynaecomastia)
- a general lack of enthusiasm or energy
- difficulty sleeping an/or or increased tiredness
- night sweats
- hot flashes
- poor concentration and short-term memory challenges.
Many men will experience male menopause symptoms in their midlife, starting in their late 40s and 50s.
For true diagnosed andropause, caused by low testosterone levels, the treatment is testosterone replacement therapy (TRT). Many men experiencing andropause symptoms, however, are not actually low in testosterone. In these cases, lifestyle changes such as improving diet, sleep, and exercise habits as well as treatment for any anxiety, stress or depression will help manage or even correct the symptoms.
Yes, they can be. They may be caused by low testosterone, but more commonly they result from anxiety and/or stress, medication side-effects, alcohol consumption, diet, or a side effect of sleep apnea.
Yes, they can be. They may be caused by low testosterone, but more commonly they result from anxiety and/or stress, medication side-effects, alcohol consumption, diets, or a side effect of sleep apnea.
[1] https://www.forbes.com/health/mind/midlife-crisis/
[2] Infurna FJ, Gerstorf D, Lachman ME. Midlife in the 2020s: Opportunities and challenges. Am Psychol. 2020 May-Jun;75(4):470-485. doi: 10.1037/amp0000591. PMID: 32378943; PMCID: PMC7347230.
[3] https://www.webmd.com/men/features/mens-midlife-crisis
[4] https://psychcentral.com/lib/midlife-crises-affecting-men-and-families
[5] https://www.nhs.uk/conditions/male-menopause/
[6] Singh P. Andropause: Current concepts. Indian J Endocrinol Metab. 2013 Dec;17(Suppl 3):S621-9. doi: 10.4103/2230-8210.123552. PMID: 24910824; PMCID: PMC4046605.
[7] https://www.webmd.com/men/guide/male-menopause
[8] https://www.merithealthcentral.com/health-library/128
[9] https://www.ucsfhealth.org/conditions/erectile-dysfunction
[10] https://www.mayoclinic.org/diseases-conditions/erectile-dysfunction
[11] https://my.clevelandclinic.org/health/drugs/10053-vacuum-constriction-devices
[12] https://www.urologyhealth.org/urology-a-z/e/erectile-dysfunction-(ed)
[13] https://www.merckmanuals.com/en-ca/home/men-s-health-issues/sexual-dysfunction-in-men/decreased-libido-in-men
[14] https://www.mayoclinic.org/healthy-lifestyle/sexual-health/expert-answers/loss-of-sex-drive
[15] https://my.clevelandclinic.org/health/diseases/24515-male-pattern-baldness-androgenic-alopecia
[16] https://www.aad.org/public/diseases/hair-loss/
[17] Aukerman EL, Jafferany M. The psychological consequences of androgenetic alopecia: A systematic review. J Cosmet Dermatol. 2023 Jan;22(1):89-95. doi: 10.1111/jocd.14983. Epub 2022 Apr 25. PMID: 35403805; PMCID: PMC10084176.
[18] Dhami L. Psychology of Hair Loss Patients and Importance of Counseling. Indian J Plast Surg. 2021 Dec 31;54(4):411-415. doi: 10.1055/s-0041-1741037. PMID: 34984078; PMCID: PMC8719979.
[19] Would you risk a breakdown to cure baldness? John Phillips. 1843 magazine, April 2024
[20] Pillai JK, Mysore V. Role of Low-Level Light Therapy (LLLT) in Androgenetic Alopecia. J Cutan Aesthet Surg. 2021 Oct-Dec;14(4):385-391. doi: 10.4103/JCAS.JCAS_218_20. PMID: 35283601; PMCID: PMC8906269.
[21] https://www.healthline.com/health/what-causes-night-sweats-in-men#common-causes
[22] https://www.healthline.com/health/mens-health/hot-flashes-men#symptoms
[23] https://www.healthline.com/health/cbt-techniques
[24] https://www.nimh.nih.gov/health/topics/anxiety-disorders#part_2225
[25] https://www.psychologytoday.com/ca/basics/anger
[26] https://www.medicalnewstoday.com/articles/cognitive-restructuring
[27] https://mantracare.org/therapy/anger/anger-management-counseling
[28] Nandy PR, Singh DV, Madhusoodanan P, Sandhu AS. Male Andropause : A Myth or Reality. Med J Armed Forces India. 2008 Jul;64(3):244-9. doi: 10.1016/S0377-1237(08)80105-0. Epub 2011 Jul 21. PMID: 27408157; PMCID: PMC4921612.
[29] Bhasin S, Valderrábano RJ, Gagliano-Jucá T. Age-Related Changes in the Male Reproductive System. [Updated 2022 Feb 10]. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK278998/
[30] https://www.mayoclinic.org/healthy-lifestyle/mens-health/in-depth/male-menopause/art-20048056
Original content, last updated February 20, 2025.
© 2025 Herstasis® Health Foundation