What are Perimenopausal Bleeding Issues?
Monthly bleeding is a fundamental part of the menstrual cycle. The lining of the uterus thickens during your monthly cycle as it prepares to receive and nourish a fertilized egg. If no egg implants into the uterus, then the whole lining inside the uterus is shed through the vagina and out the vulva, resulting in a monthly flow of menstrual blood.
This process is completely driven by hormones, so it is not surprising that the variability in hormone levels during the menopausal transition impacts this monthly cycle and affects the regularity, heaviness, quality, and length of menstrual bleeding. Any of these issues, alone or in combination, can have a significant impact on a woman’s quality of life.
Perimenopause is the time when a woman transitions out of her reproductive years, ending in menopause when periods and ovulation have completely stopped for a full 12 months in a row. One of the hallmark symptoms of the menopausal transition is changes in the bleeding associated with your menstrual cycle. Commonly, the length and timing of the menstrual cycle become irregular, even to the point of getting a period every 2 weeks during perimenopause. Other changes include differences in the appearance and volume of menstrual blood. [1]
Experiencing vaginal bleeding after menopause (12 months without a period), or bright red heavy bleeding after menopause is not normal. Spotting after menopause is less concerning, although if it is frequent or becomes a flow it could be a problem. In any of these cases, see your healthcare provider.
During the menopausal transition, your estrogen and progesterone levels are highly variable. These fluctuations vary from month to month and are often erratic, impacting ovulation and the rest of your menstrual cycle. This can be experienced as irregular or missed periods, as well as changes to your ‘typical’ menstrual bleeding.
Heavy periods can be identified by:
- ▢ Needing to change your pad or tampon every hour
▢ Bleeding that goes on for more than seven days
▢ Bleeding (not spotting, but proper menstrual flow) happens more frequently than every 3 weeks
▢ Menstrual flow that contains blood clots larger than the size of a quarter.

See your healthcare provider if you have:
- ▢ Any concerns about your bleeding
▢ Extremely heavy bleeding (when you need to change your pad or tampon every hour)
▢ Bleeding that goes on for more than seven days
▢ Bleeding (not spotting, but rather a menstrual flow) that happens more frequently than every 3 weeks
▢ Menstrual flow that contains blood clots larger than the size of a quarter.
This heavy bleeding is called menorrhagia. You will likely have a pelvic exam, blood tests, and possibly an ultrasound, all of which are used to rule out serious problems. [2]
Getting a proper diagnosis requires ruling out other possible reasons for your heavy bleeding.
◇ A pap test will rule out cancerous growths, infection or inflammation
◇ An ultrasound may be used to check for fibroids in the uterus
Based on the results from those tests, you may get a biopsy, which is a tissue sample from the uterine lining or a hysteroscopy, which uses a small camera inserted through the vagina to directly examine the cervix and the inside of the uterus. Finally, you may require a procedure known as a dilation and curettage (D&C), where the lining of the uterus is scraped away so the inside of the uterus can be examined. [2] [5]
Self-Care & Natural Remedies for Menopause Bleeding Issues
Getting used to changing menstrual periods can be a challenge and can be frustrating. Anemia is a condition where you are low on red blood cells causing fatigue and weakness. In perimenopause this can happen from losing too much blood due to heavy bleeding. To manage anemia you may increase iron-rich foods in your diet, including red meat, spinach, lentils, and eggs.
You may also try the following supplements on the advice of your healthcare provider:
-
➜ iron supplements
➜ folic acid supplements (used in the formation of red blood cells) and/or
➜ vitamin B12 supplements (which help the body produce healthy red blood cells)
You can also practice meditation and/or breathing exercises, which won’t impact your bleeding but can improve your quality of life and make managing your bleeding easier.
There are a few things you can do to help manage your experience:
Therapies & Treatment for Bleeding Issues
At age 40 find a reliable, educated primary care provider familiar with recognizing and treating symptoms of perimenopause and menopause. The North American Menopause Society provides a list of menopause practitioners here.
Bleeding issues such as changes in length of flow, heaviness of flow, and changes in colour and texture of blood are almost certain to happen as you move through the menopause transition towards menopause. Despite this, changes in your usual bleeding patterns can be a sign of other, more serious, problems such as abnormal growths inside your uterus (called endometrial hyperplasia). [1]
Treatment Options

Oral Contraceptives
Oral contraceptives are a common medical treatment for very heavy periods, however, they may not be effective to treat menorrhagia.

NSAIDs
Prostaglandin inhibitors are nonsteroidal anti-inflammatory drugs (NSAIDs), including aspirin or ibuprofen. They may be helpful in reducing the amount you bleed and can also be helpful for cramping.

IUD
An Intrauterine Device (IUD) that releases progestin has been shown to be a more effective therapy, and can be prescribed to treat heavy bleeding for up to five (5) years. [2][6]
If these approaches do not help your heavy bleeding, other medical treatments to explore with your doctor or healthcare provider include endometrial ablation (surgical removal of the uterine lining), a hysterectomy, and/ or surgical removal of any fibroids or cysts in the uterus or ovaries. [2] [5]
The Science
Among women in the early menopause transition, abnormalities in timing of menstrual bleeding – both changes in the length of your cycle or changes in the number of days you typically bleed – are the result of changes in hormone levels. These changing hormones also result in anovulation, cycles where you do not ovulate, or release an egg.
Abnormally heavy periods, however, do not appear to require hormonal fluctuations. In some studies, heavy periods are more closely associated with obesity (a body mass index (BMI) of 30 and above) and the presence of benign fibroids (leiomyomata). Heavy periods are less likely after anovulatory cycles where no egg was released. [2]
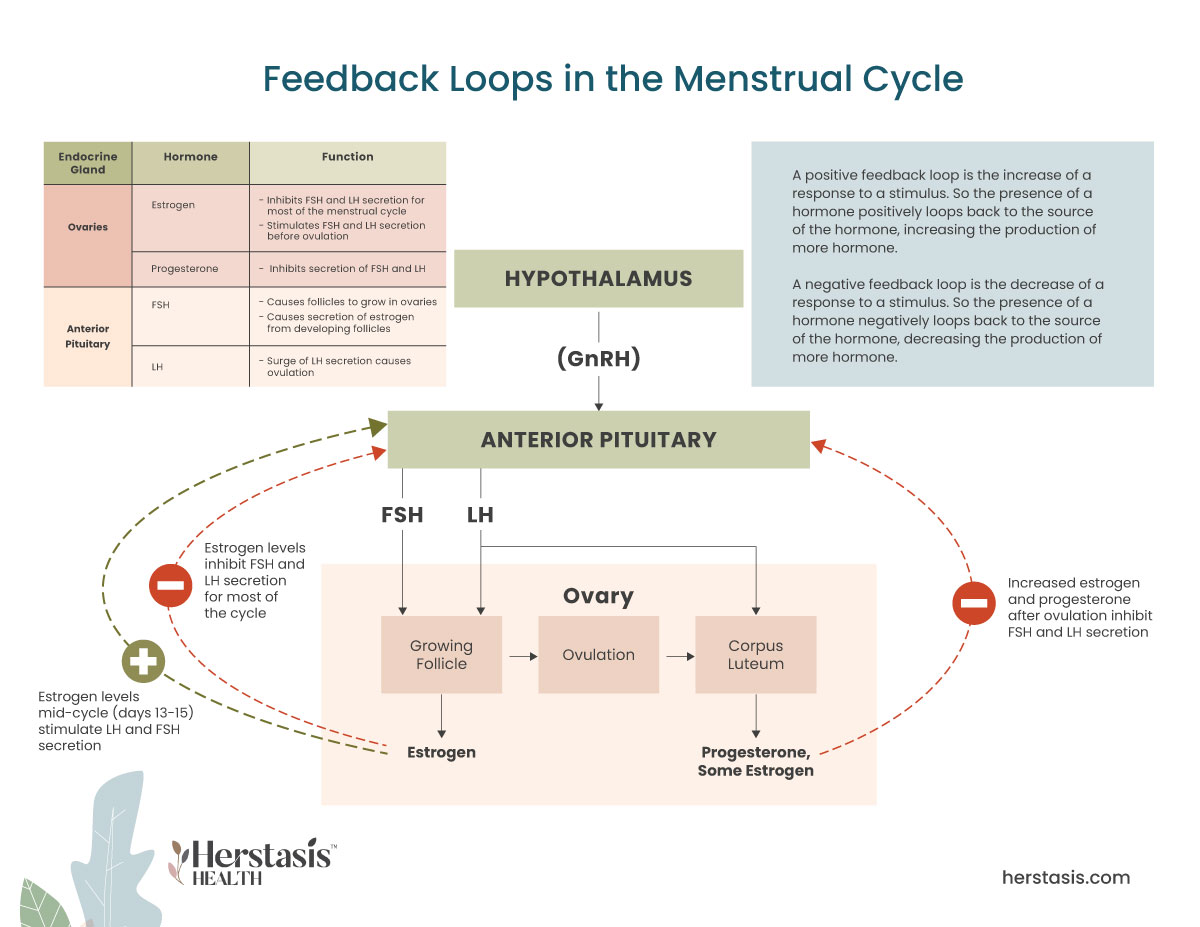
The different hormonal and physical processes driving your menstrual cycle. [5]
The menstrual cycle involves the monthly release of an egg from one of the ovaries, a process called ovulation. The uterus prepares to receive a fertilized egg via a series of hormonal changes. If the egg does not get fertilized by a sperm cell then the lining of the uterus isn’t needed and it is shed through the vagina – resulting in a menstrual period. [4]

This menstrual cycle is driven by changes in hormones, particularly estrogen, progesterone, luteinizing hormone (LH) and follicle-stimulating hormone (FSH). Estrogen and progesterone are called ‘sex hormones’ because they are secreted by your ovaries, which are the female sex organs. LH and FSH are gonadotropins because they are secreted from cells in the anterior pituitary called gonadotrophs (gonads are the formal term for the sex organs – ovaries in females, and testes in males).
There are three stages in the menstrual cycle: the follicular stage (before release of the egg); the ovulatory stage (egg release); and the luteal stage (after egg release).
At the end of the luteal phase, if the egg isn’t fertilized, the corpus luteum breaks down and stops producing progesterone. Estrogen levels also decrease. This causes the top layers of the uterine lining to break down and begin shedding, starting menstrual bleeding and the beginning of a new menstrual cycle. [4] [5]
When you have not had a period for one full year (12 months), you have officially entered menopause.
The most common reason for spotting after menopause is hormonal imbalance. This can be caused by a variety of factors, including changes in diet, stress levels, and medications. Other potential causes of spotting after menopause include uterine fibroids, endometriosis, and ovarian cysts. In rare cases, spotting after menopause may be a sign of cervical or endometrial cancer.
During perimenopause, the time before the period ceases, it is normal for women to experience bleeding that is heavier than usual. This bleeding can last for a few days to a few weeks. In some cases, the bleeding may be so heavy that it interferes with a woman’s daily activities. If this occurs, it is important to see a doctor to determine the cause of the heavy bleeding.
The answer to this question is not entirely clear. There is some evidence that heavy bleeding may occur before menopause, but the research on this topic is still relatively limited. It’s possible that heavy bleeding may be a symptom of perimenopause, which is the transition period leading up to menopause. During perimenopause, hormone levels fluctuate and can cause changes in the menstrual cycle, including longer or shorter periods, or heavier or lighter bleeding.
The most common reason for spotting after menopause is hormonal imbalance. This can be caused by a variety of factors, including changes in diet, stress levels, and medications. Other potential causes of spotting after menopause include uterine fibroids, endometriosis, and ovarian cysts. In rare cases, spotting after menopause may be a sign of cervical or endometrial cancer.
NOPE, not true at all.
The blood that leaves your body during menstruation isn’t toxic, and it isn’t ‘bad’ in any way. Rather it is a normal, healthy result of your menstrual cycle. Menstrual blood will not interfere with your sexuality and it does not mean you are unclean in any way.
FALSE
Birth control pills are often used to manage menstrual blood flow and are commonly prescribed for heavy bleeding. Older versions of birth control pills did have high doses of estrogen, which increased the risk of blood clots in women over 35, however today’s birth control pills use much lower doses of estrogen and do not carry the same risks. In fact, today’s birth control pills are known to have benefits that include a lower risk of ovarian and endometrial cancer. Birth control pills are not recommended for women over 35 who smoke, have high blood pressure, or have a history of heart disease.
YES
There are several treatment options available, some of which, like a hormonal IUD, can be used to treat heavy periods for up to five years. Talk to your healthcare provider to find the best solution for you.
YES
Heavy bleeding and/or long menstrual periods can lead to health issues including iron deficiency anemia (IDA). As well, heavy bleeding can have a major negative impact on a woman’s quality of life because it can interfere with daily activities.
NO
Not true. Heavy bleeding during the menopausal transition is linked to obesity and fibroid tumours. If you experience heavy bleeding and are not in the menopausal transition, talk to your healthcare provider to rule out any serious health issues.
FALSE
Heavy periods that involve losing more than 80mL of blood (5.5 tablespoons) are not normal. This condition is called menorrhagia and current research suggests they are not totally hormonally driven. Rather they are also linked to obesity and/or the presence of fibroids (fibroid tumours). [5]
[1] Van Voorhis BJ, Santoro N, Harlow S, Crawford SL, Randolph J. The relationship of bleeding patterns to daily reproductive hormones in women approaching menopause. Obstet Gynecol. 2008 Jul;112(1):101-8. doi: 10.1097/AOG.0b013e31817d452b. PMID: 18591314; PMCID: PMC2666050.
[2]https://www.healthline.com/health/menopause/perimenopause-periods
[3] https://www.webmd.com/women/news/20130104/iud-heavy-menstrual-bleeding
[4] Anne Firquet,Wolf Kirschner &Johannes Bitzer. Forty to fifty-five-year-old women and iron deficiency: clinical considerations and quality of life. Gynecological Endocrinology. 2017; 33 (17):503-509
[5] https://www.hopkinsmedicine.org/health/conditions-and-diseases/menorrhagia
[6] Gupta J., Kai J., Middleton L.; Pattison H., Gray R., and J. Daniels Levonorgestrel intrauterine system versus medical therapy for menorrhagia. N Engl J Med. 2013; 368: 128-137
Original content, last updated February 6, 2025.
© 2025 Herstasis® Health Foundation














